Education guide

While both nurse practitioners and physician assistants can work in the same health care field, PAs are usually licensed and can operate their own practice. NPs must be supervised by a licensed physician. PAs finish school faster than NPs, and they can practice in almost any field. Both have similar educational requirements, but PAs can practice in a variety of different settings, including the private sector.
But, if you want to make a difference in the healthcare industry, be sure to take a closer look at the benefits of each.
Nurse Practitioner vs Physician Assistant: What’s the Difference?
| Nurse Practitioner (NP) | Physician Assistant (PA) | |
| Duties | NPs are health care providers that can prescribe medication, examine patients, order diagnostic tests, diagnose illnesses, and provide treatment, much like physicians do. In certain states they can work independently from a physician. | PAs have the ability to treat patients independently of a medical physician. They perform a variety of duties including writing prescriptions, ordering and interpreting laboratory tests, assisting in surgery, performing minor bedside procedures, diagnosing patients, developing treatment plans, and obtaining patient histories. |
| Salary | $111,680 / year | $115,390 / year |
| Education | Master’s degree | Master’s degree |
| Program Costs | $35,000 – $70,000 | $60,000 to $90,000 |
| Scope of Practice | Can operate own practice in certain states. | Can operate own practice in certain states. |
| Career Outlook | 45% predicted career growth from 2019-2029 | 31% predicted career growth from 2019-2029 |
| Certification | NP recertification is every two years and requires a minimum of 1,000 clinical hours in your certified specialty and continuing education hours. | PA recertification is two parts. Every two years, 100 continuing education hours are required and every ten years a recertification exam must be passed. |
NPs can practice in nearly any field
Nurse practitioners practice in many different fields, including emergency medicine, family medicine, and pediatrics. They may also work in telehealth settings, answering insurance companies’ nurse helplines. The scope of practice of an NP has also expanded. In most states, they can work in almost any specialty, so it is not uncommon for them to work in the same field as a physician. However, this new practice model may put some doctors off.
Although the majority of states have made the full-practice-authorization law available to NPs, they are not yet licensed to practice independently. Some payers still limit the scope of practice of NPs to certain sites, and others prohibit them from practicing independently. As a result, NPs may not practice independently in all locations.
The National Academy of Medicine and the National Council of State Boards of Nursing recommend that nurse practitioners practice the full scope of their training. However, many professional organizations and state boards have been working to remove barriers to NP practice. The American Association of Nurse Practitioners (AANP) and the American College of Nurse Practitioners (ACNP) have both been working to eliminate regulatory obstacles.
While FNPs and ANPs are often confused, both have similar training. The primary difference is that FNPs tend to focus on the prevention and restoration of health, while PAPs tend to look at the underlying pathology and cure of a patient’s problem. This makes nurse practitioners highly valuable in the care of aging patients. It is also important to note that NPs may work under a collaborative practice agreement.
The NP profession has several advantages. For one, it is patient-centered and requires constant innovation to meet the needs of society and the latest advancements in health care science. The NP role allows the practitioner to combine the roles of provider, educator, researcher, and advocate, and participate in health policy activities. The NP role is growing in the United States as the healthcare costs continue to spiral out of control.
PAs can operate their own practice
Many states have made it easy for PAs to practice independently, and Alaska is one of those states. This state has more PAs per capita than any other, improved PA practice laws, and a friendly regulatory environment. It also has one of the highest salaries of all states for PAs. Other states that allow PAs to practice independently include Illinois, Ohio, and South Dakota, which limit the ratio of PAs to physicians and restrict PAs’ prescription authority.
In order to operate independently, PAs must meet certain qualifications set by state statute. Any PA who fails to meet these requirements can be charged with negligence or medical malpractice. PAs must always be available for questions from patients and physicians, since the physician is the “legal master.” In addition, PAs can buy malpractice insurance to protect themselves from any lawsuits that may occur during their practice. There are various PA associations that offer malpractice insurance.
Some states allow PAs to operate their own practice, but their scope of practice may differ from that of NPs. In Wyoming, for example, PAs can complete a medical certification of death form and prescribe opiate antagonists for patients at risk of opioid overdose. While federal law does not require employers to provide breaks for PAs, many states do. The key is to find a state that allows PAs to operate their own practice.
Physician assistants can run their own medical practice if they possess the training, the necessary licensing requirements, and access to the appropriate funding sources. In California, for example, physician assistants are allowed to establish a professional corporation. To operate a practice, PAs must own 51-100% of the corporation. In addition, they must employ a supervising physician. They are responsible for all aspects of their practice, including patient care, billing, and ensuring quality patient care.
If you are thinking about starting your own practice, consider hiring a PA and NP to share the call burden. Be sure to negotiate your call schedule ahead of time, and consider adding a satellite office to reach a wider clientele. By adding a PA or NP to your practice, you’ll be able to increase your hours and improve your patients’ care. During the day, you’ll be able to address your patients’ questions while the NPs or PAs are on the clock.
NPs must be supervised by a licensed physician
According to the Institute of Medicine and the National Council for State Boards of Nursing, NPs should be given full practice status, although most states have limited regulations for this. Depending on state regulations, NPs may be allowed to treat patients independently, but must be supervised by a physician. In some states, the scope of practice of NPs is restricted, while in others, they are permitted to prescribe and administer medications only under the direct supervision of a physician.
Under the New York State Education Law, NPs are required to work under the supervision of a licensed physician. In New York State, this relationship should be collaborative, meaning that the NP is responsible for communicating with the physician and is not an independent practitioner. The New York State Education Law also prohibits fee splitting, kickbacks, and other types of financial relationships between a physician and an NP.
The number of states that require the supervision of NPs varies, with nine states requiring a physician to review the patient’s chart; 42 states do not. While physician assistant record review requirements vary by state, they tend to be less rigorous than those for physicians. In general, this supervision requirement is about 10 to 20% of patient charts. Additionally, some states place additional terms to govern the relationship between the physician and NP. For example, in Georgia, a physician may enter a supervision agreement with up to eight NPs, but may only actively supervise four at a time. Other states have different limitations depending on whether an NP is a part-time or full-time employee.
The PPP is attempting to help AMA change the regulatory tide by providing education to the public and legislators about the role of nurse practitioners. It focuses on truth, transparency, and patient safety in healthcare. Although the AMA has not adopted any formal guidelines on physician supervision of NPs, it has approved several recommendations for NPs to work under the supervision of a physician. If a physician licensee agrees to the recommendations, this is the best way to ensure safe care.
PAs finish school faster than NPs
As the demand for healthcare providers grows, the number of physician assistants is projected to increase by 31% over the next decade. Although physician assistants are able to complete school and become practitioners faster, they also face a steep learning curve. Here are some differences between physician assistants and nurse practitioners. Both types of medical professionals have a range of practice settings. For instance, physician assistants can specialize in pediatrics or internal medicine, while nurse practitioners can specialize in any field.
One difference between NPs and PAs is certification. NPs must be licensed at the state level and participate in continuing medical education. While PAs are not required to complete residency programs, they must pass the PANCE exam to gain licensure. Nurse practitioners must also maintain a license while practicing, but PAs need only hold an active one. They can work in all areas of healthcare, including hospitals, community clinics, VA facilities, and nursing homes.
In addition, physician assistants and nurse practitioners are largely equivalent when it comes to training. Both require a master’s degree and must be licensed in their states. While nurse practitioners and physician assistants have similar job descriptions, PAs typically hold doctoral degrees. Nurse practitioners have more advanced educational backgrounds and can work independently and collaboratively with physicians in a medical practice. However, PAs are allowed to see more patients and are more effective at treating a specific patient population.
Although nurse practitioners tend to be more educated than nurse practitioners, both fields have a high demand for medical professionals. PAs are expected to grow at a faster rate than nurse practitioners. On the other hand, nurse practitioners may need to earn more than their NP counterparts. For example, nurse practitioners tend to earn more than twice as much as NPs, but this difference is negligible if the person’s background is in the medical field.
Aspiring physician assistants must obtain a bachelor’s degree. Most programs require a Bachelor of Science in Health Sciences, although some graduate programs may accept graduates with other bachelor’s degrees. For the Master’s degree, a candidate should have a 3.25 GPA in all relevant courses. Some programs may require that the candidate have some work experience before applying. A few schools offer dual BS/MS physician assistant programs. This option saves time.
RECOMMENDED TOPICS
- JAMB 2025 UTME/DE registration document – step-by-step on how to apply for UTME and DE
- JAMB postpones 2025 UTME Registration to February 3rd

- JAMB Officially Announces 2025 UTME Registration, Exam, Mock Dates, Cost and Important Details

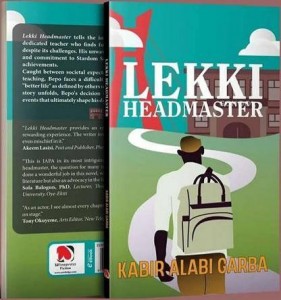
- The official reading novel for Jamb 2025 is Lekki Headmaster
- Subjects for Computer Science in JAMB for Guaranteed Success


